Neuroblastoma Parent Global Symposium 2022 Round-up
Welcoming over 400 participants from across the globe, last month we returned with the third edition of the Neuroblastoma Parent Global Symposium - and what an event it was!
Here’s a look back on the sessions at NPGS 2022 and what we've learnt...
Setting the scene
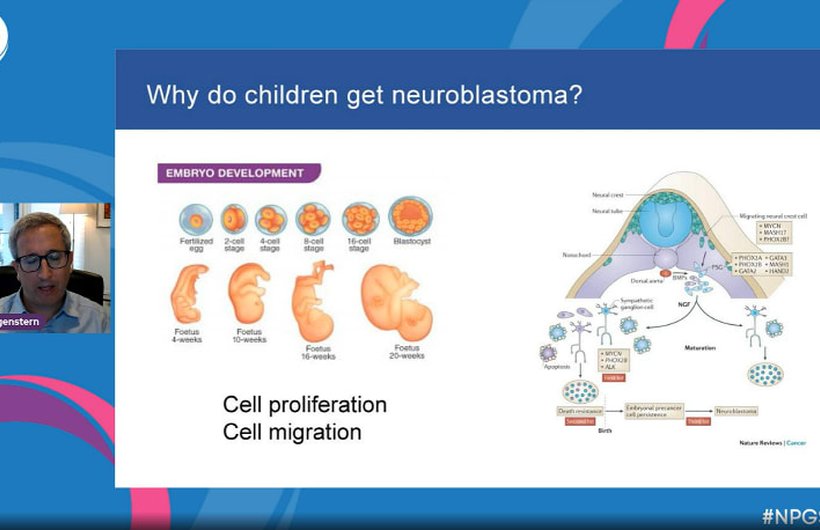
Returning once again to the NPGS stage, Dr Daniel Morgenstern hosted this year’s symposium, giving a warm welcome to our global audience.
His opening talk gave an introductory overview of neuroblastoma to provide a useful basis for those new to the topic, and context behind the research-focused sessions to follow.
The next session, The challenge of curing high-risk neuroblastoma, built on this basic knowledge to give an idea of the themes of research currently being progressed in neuroblastoma.
Is precision the way forward?
One of the major issues with treatment for high-risk neuroblastoma is that it is incredibly invasive, multi-modal and toxic due to the wide variation in disease case-by-case. This means very high exposure to harmful therapies, as there is a need to ‘throw everything possible’ at the cancer to get rid of it.
A theme that ran across this session was how to move towards a future where treatment is much more tailored to the individual's needs. This could mean exposure to less therapies where we know they won’t be effective, as well as introduction of precision medicines for sub types of disease with certain attributes. One vital part of developing this approach is to be able to characterise a child’s disease and identify the right therapeutic targets. Prof Jan Molenaar presented the work of the Princess Maxima Centre in The Netherlands on molecular profiling and mass screening of early therapeutic agents which helps the global research community to prioritise areas in which to work.
Taking a personalised approach to treatment is also prevalent in cases of relapsed and refractory neuroblastoma, where there is often no standard pathway to follow. One of the options being investigated for these patients is to receive extended induction chemotherapy where the standard backbone is supplemented with ‘bridge’ therapy. Dr Sara Federico presented results from a study on this, which shows that this could be an effective pathway for some patients, depending on previous treatment and extent of relapse.
In Dr Rajen Mody’s talk on chemoimmunotherapy, he explained the work taking place to help capture data on these personalised approaches that are taken outside of clinical trials. This is a very important venture in the field as it is common for children with cancer to receive compassionate or ‘off-label’ therapies where they have little other options. The material he presented showed a promising correlation between the effectiveness of chemoimmunotherapy in both clinical research and ‘real-world’ use.
Dr Steve DuBois closed this session with an outlook on the work being done to improve frontline treatment for high-risk neuroblastoma - including the move towards targeted therapies. The ongoing Phase III trial in the US, ANBL1531, is looking to consolidate innovations in induction treatment including MIBG therapy, ALK inhibitors and Anti-GD2 therapy through a multi-arm study that will assess the success of these new approaches across a range of cases of neuroblastoma with different characteristics.
Cutting edge research
Next on the agenda was the session on CAR T-cell therapy. This area of research is well established in other specific cancers, including leukaemia, but is still being developed for use in solid tumours including neuroblastoma. Our panel of speakers spoke about this emerging science and what must be considered as this specialism moves forward...
CAR T-cell therapy- what is it all about?
Prof John Anderson answered this question in his opening to this session, explaining that CAR T cells are antibody cells that are taken from the patient, then genetically engineered to boost their cancer killing abilities, before being put back into the patient’s system. He also gave an overview of the advantages and issues of this type of technology, and ideas on how we might develop to overcome these.
How can we make them work for neuroblastoma?
The research presentations by Dr Andras Heczey, Dr Mark Yarmarkovich and Dr Rosa Nguyen detailed some of the approaches being taken to optimise this mode of treatment for solid tumours.
Natural Killer T-cells (NK T-cells) are an alternative to standard T-cells that may be a better option to explore. As hinted by their name, these cells can naturally target and kill tumour cells more effectively, which could boost activity in solid tumours. This is what was presented by Dr Heczey, alongside results from the Phase I study in the US that showed effective absorption of CAR NK T-cells into neuroblastoma tumours, as well as encouraging initial results on their effectivity at killing tumour cells. Now that safety and initial efficacy have been assessed, this work will move forward to develop this experimental technique further.
Another factor in improving the effectiveness of CAR T-cell therapy is choosing the right targets on tumour cells. PHOX2B is one target being explored in Dr Yarmarkovich’s work. It appears on the surface of neuroblastoma cells, but is also linked to cancer drivers within the cell centre. This means that targeting PHOX2B could help to overcome one of the drawbacks of CAR T for solid tumours which is that it we can only target the cell surface. Dr Rosa Ngyen introduced another target under investigation - GPC2. This is a molecule on the cell surface that drives neuroblastoma progression and growth. Preclinical work in her group has shown that with optimisation, CAR T-cells could be developed to effectively destroy tumour cells by targeting GPC2.
Can we take Anti-GD2 therapy further?
This was the question at hand in our Special Interest talk: ‘Anti-GD2 antibody therapy: an important approach in the treatment of neuroblastoma’. Many will be familiar with anti-GD2 immunotherapy which is part of the standard frontline treatment pathway for high-risk neuroblastoma in a number of countries including the UK. Here it is used as maintenance therapy which helps to keep a child in remission at the end of their treatment. Research is now looking to see where anti-GD2 therapies might be effective in actively killing neuroblastoma cells, especially where standard modes of treatment like chemotherapy don’t work.
Dr Robbie Majzner opened the session with his work on anti-GD2 combination strategies for relapsed and refractory disease. One combination is that of anti-GD2 and anti-CD47 agents which aim to boost the immune system to kill cancer cells more effectively. The Phase I study of this combination led by Dr Majzner has proven both safety and promising efficacy of this combination. The group are now moving forward to combine these further with low-doses of chemotherapy to improve efficacy even further, a project we are excited to be working on with him in this preclinical study funded through our 2019 RFA.
What does it mean for the clinic?
Bringing the clinical perspective on anti-GD2 was immunotherapy expert Dr Juliet Gray. There have been a number of studies to improve the use of anti-GD2 as a maintenance therapy which has helped to mitigate some of the drawbacks including severe pain. This continued research has also led to the discovery of promising pathways which are now being investigated in the BEACON Immuno and MiNivAn studies, led by Dr Gray in the UK and funded by Solving Kids' Cancer UK. These late-phase trials are again looking at combination therapies that incorporate chemotherapy and immunotherapy, and the initial results presented are indicating that this continues to be an important area to explore, especially in cases of relapse or refractory disease.
Life beyond treatment
Empowering parents throughout the whole of their experience of neuroblastoma is vital, and this often goes beyond treatment, trials and research. In our Special Interest talk: ‘Post Treatment- A Parent Perspective’, Family Support Coordinator and Mum to Eva, Hayley Blackwell, presented a safe space for parents facing the emotional challenges of life post-treatment. From feeling forgotten, to back-to-school anxiety and survivor guilt, the session opened up conversation on some of the less-talked about struggles faced by families in remission. Sharing the experiences of other parents as well as her own, Hayley also shone a light on the significance of late effects after treatment, the impact that these have on both the child and family, and how this support in this area could be improved.
This insightful talk led to a very open and honest discussion from our parent panel, who covered audience questions including how to talk to your child about their experience, support from schools for children post treatment, and healing as a family.
All of the sessions from this years NGPS event can be accessed on demand on the page below, alongside the full library of previous NPGS resources.
Neuroblastoma Parent Global Symposium
Learn more about our virtual education symposium for parents and extensive NPGS video library.
 Read more
Read more